“Had I been able to bring my parents here, things would have been very different. Now, they’re fighting for their lives,” lamented Rahul — an American who grew up in Delhi, India and now lives in Seattle, Washington — to Vox. When Rahul’s 74-year-old father contracted COVID-19, he embarked upon a difficult journey of recovery. Rahul’s mother remains on a ventilator in the intensive care unit at an Indian hospital where the overwhelmed hospital staff, almost all of whom remain without access to vaccines, struggle to directly inform Rahul of his mother’s condition. As a result of the U.S. travel ban on India, Rahul may never see his mother alive again.
Meanwhile, the electric beat of “Ice Ice Baby” and “MMMBop” soars out into the bustling sidewalk of the Chelsea area of Manhattan, New York. Just one year ago, these streets were lined with refrigerated morgue trucks and exhausted health care workers covered head-to-toe in PPE. But now, it’s ’90s night at Rumi, a club filled to capacity with millennials and Gen Zers clad in themed costumes and carrying laminated vaccination cards. Drinking, dancing, and singing fill the ballroom, where patrons relax unmasked in a designated lounge space, seemingly from another era of carefree normalcy.
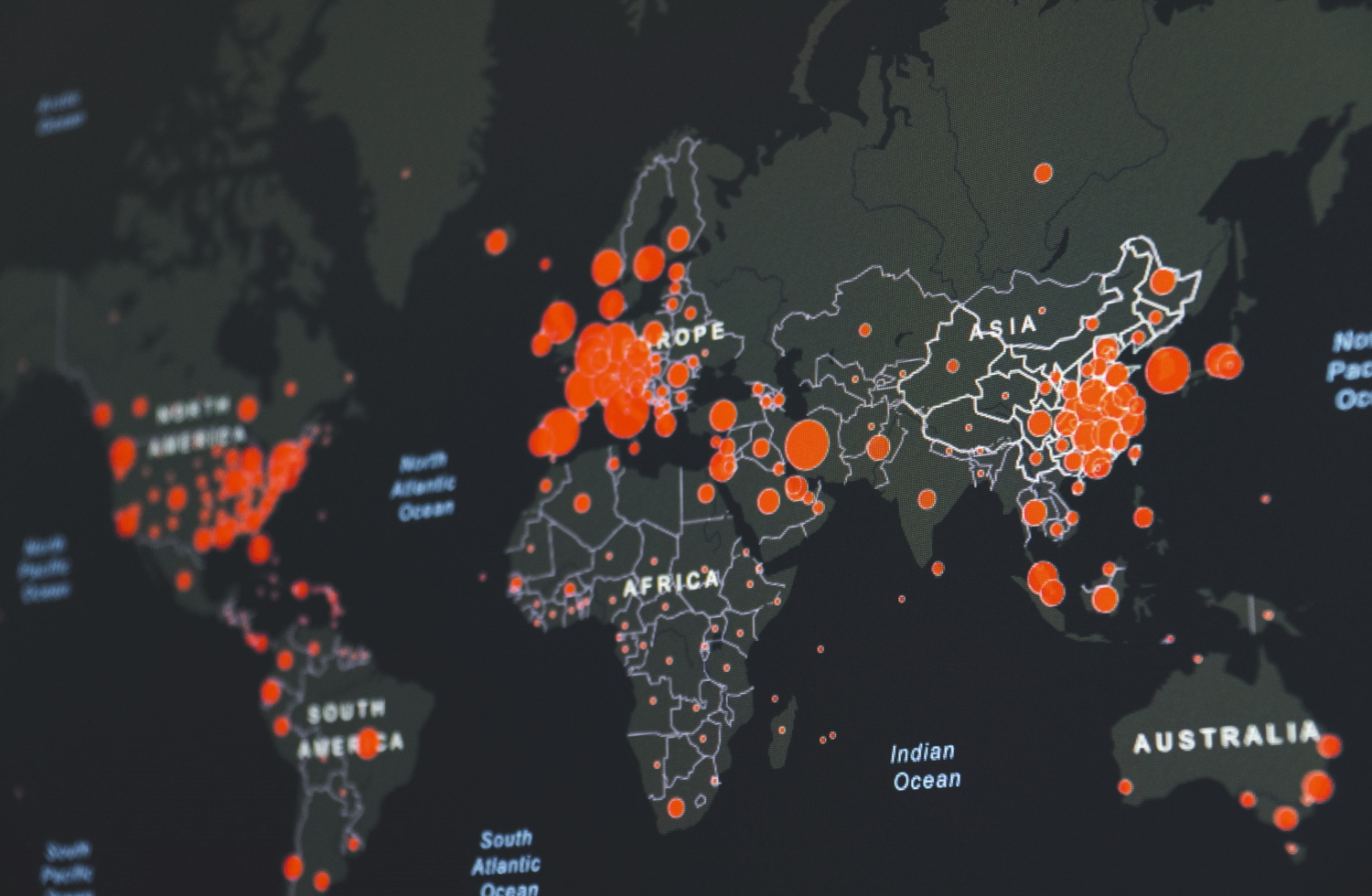
The COVID-recovery divide between India and America did not arise by accident. Today, wealthy countries like the United States are on the fast track to normalcy because they have stockpiled enormous vaccine surpluses before lower-income nations could access the global vaccine market. As a result, lower-income nations still struggle to gain access to vaccination, even for health care workers. With U.S. vaccination rates slowing down, it is America’s moral obligation to quickly share its surplus with the rest of the world to prevent the spread of infection, diminish the potential for variants to arise, and ensure that lower-income countries have equitable access to COVID-19 vaccines. The United States federal government must immediately accelerate donations of its excess vaccine supply to other countries with greater need.
A Gamble That Paid Off (for Some)
In May 2020, the United States government paid $1.2 billion to AstraZeneca, a British drug manufacturing company, to help accelerate their research to develop a COVID-19 vaccine. In return, AstraZeneca agreed to give the United States 300 million doses of their vaccine if it passed safety and efficacy tests. The United Kingdom also struck a similar deal with AstraZeneca to acquire 90 million doses of their vaccine in exchange for providing research funding.
Throughout 2020, numerous wealthy nations like Japan, Canada, the United States, and the United Kingdom spent billions of dollars to secure millions of vaccine doses for their respective countries through such bilateral agreements. By inundating drug manufacturers like Pfizer, BioNTech, and Moderna, AstraZeneca with billions of dollars in funding, these nations helped fund the research that brought multiple effective COVID-19 vaccines to market in record time; however, this funding only reserved vaccines for the countries wealthy enough to provide research funding for months during the height of the pandemic.
By January, 96% of Pfizer/BioNTech vaccines and 100% of Moderna’s doses scheduled to be produced by the year’s end had already been purchased. Before the pandemic reached its height, countries with 16% of the world’s population had a monopoly over half of all available vaccine doses. Today, while the virus continues to ravage countries like Brazil and India, pushing their health care systems towards collapse, the United States and other wealthy countries that bought millions of vaccines in advance of production are on the road to normalcy.
This blatant inequity in vaccine availability is not only lengthening the pandemic but also allowing new variants to arise and contributing to an onslaught of preventable deaths internationally. Ironically, the deals that enabled the vaccines to exist in the first place are now exacerbating the pandemic by making vaccination harder to access for most of the global population.
Inequity Inherent in the Process
Wealthy nations took a major risk by making deals with drug companies to secure vaccine doses prior to manufacturing. Since these countries had no guarantee that the billions of dollars they spent to fund research would yield a vaccine approved as safe and effective, each nation made multiple such deals with several different drug companies to lower the stakes of their large investments. In doing so, rich countries frequently secured enough prospective vaccine doses to serve each member of their respective populations several times over.
For instance, by March, Canada had secured over 316 million doses, an amount sufficient to fully vaccinate their entire population five times. The United States and the European Union had also made enough deals to vaccinate their entire populations at least twice. Since poorer countries could not afford to make these kinds of high-risk investments, they were already far behind in the distribution priority by the time the vaccines were approved.
In order to address pervasive economic inequity inherent in the vaccine acquisition process, the World Health Organization, the Coalition of Epidemic Preparedness Innovations, and Gavi, the Vaccine Alliance developed a program called COVAX. This initiative aims to reduce the delay in vaccine allocation to middle and lower-income nations. Through COVAX, wealthier countries would be able to invest in a variety of vaccine developers at once on a collective basis to reduce the risk of their individual investments and diminish the potential for surplus vaccine distribution outcomes. COVAX also uses donations from wealthier countries and charities to purchase vaccines for lower-income nations. As vaccines became available, COVAX planned to distribute them to every participating country at the same time so rich countries could not jump the line.
Due to the multilateral nature of COVAX’s system, it requires participation from most countries to be effective. However, since COVAX was established in April 2020 after the pandemic had already taken root, most wealthy countries had already invested billions of dollars into bilateral agreements with drug companies, thereby reducing the incentive for these nations to participate in COVAX and diminishing its potential efficacy. As a result, despite countries like the U.S. contributing to COVAX’s funds for poorer nations, they are still at the front of the manufacturing line. Even though the U.S. and the U.K. pledged to donate vaccines to COVAX, neither nation has made an explicit commitment as to whether these donations will be repeated as necessary. With international cooperation, COVAX can serve as a viable resource to combat global health inequity in future disease outbreaks, but it is far too late for prevention this time around. COVAX faltered due to a lack of early participation from rich countries, and this disparity in vaccine access is hitting poorer countries the hardest.
A New Take on America First
Despite President Joe Biden’s strong campaign theme of breaking with the Trumpian approach to governance and leadership, regarding the COVID-19 pandemic, Biden has overwhelmingly failed to abandon Trump’s “America First” attitude. The United States is currently one of the world’s leading practitioners of vaccine nationalism, a phenomenon in which each nation prioritizes securing ample doses for its own population without consideration for the impact that such efforts will have on poorer countries that cannot afford to buy surplus vaccines en masse.
Today, the United States is in a position where it possesses millions of more doses than necessary to vaccinate its citizens. This “America First” approach to vaccination hoarding is not only unreasonable but also morally unconscionable.
The United States began to offer vaccines to 12 to 15-year-old children in May. The Biden administration has detailed a plan to vaccinate all children from 5 to 11-years-old and is considering vaccinating children as young as 2. According to health experts, “Compared with children ages 5 to 17, people ages 75 to 84 are 3,200 times more at risk of dying from COVID-19 … For children, the risk of disease is not zero, but the mortality risk is comparable to that from seasonal influenza, and hospitalizations occur in about only 0.008% of diagnosed infections.” Rich countries like the United States have started vaccinating children, but meanwhile, health care workers in many poorer nations still don’t have vaccine access at all. Dr. Seth Berkley, the CEO of Gavi noted, “It’s a natural thing … to try to protect one’s own family… But if you do that and the virus is continuing to spread in other places and mutates, then you all — not just your children but the parents themselves — can be at risk of further outbreaks.” Though American children should undoubtedly be vaccinated, sending doses abroad must be the first priority, as health care workers and elderly citizens internationally are at much higher risk than young Americans.
“I lost two uncles and one cousin on my father’s side due to the coronavirus,” a Harvard student from Brazil told the HPR. The student’s cousin was in his late thirties when he died. “All three of them passed away when some countries had already started the vaccination campaigns. Had the situation been managed properly in Brazil, I have no doubt that their lives would have been preserved … By donating doses to other countries, wealthy countries will be saving more lives and reducing the risk for unvaccinated people.”
In April, Biden committed to sending sixty million AstraZeneca vaccines to nations with greater need. However, as of September, the United States still has about 150 million surplus doses stockpiled in warehouses. Due to federal safety regulations prior to being sent abroad, experts predict that this delay will make donations far too insufficient and late. Duke researchers predicted that by July, the United States would possess more than three hundred million surplus doses, even if America kept enough shots to vaccinate most of its child population. However, as of October, the U.S. is projected to have over a billion surplus doses by the end of 2022. With this much excess, all eligible and soon-eligible Americans could get vaccinated, and the country would still have enough extra shots left over to give to every member of the U.S. population.
With a surplus this staggering, the United States can no longer afford to stockpile hundreds of millions of unnecessary doses in the name of prioritizing Americans first. Doing so would leave COVID-19 outbreaks unchecked in poorer countries, kill millions internationally, and provide time for the virus to mutate into more virulent variants.
The Recovery Divide
Today, almost 80% of American adults have at least one dose of a COVID-19 vaccine, the country is experiencing a steady decline in daily cases, and numerous Americans have returned to a life of partying, traveling, and rejoicing in the freedom of being newly vaccinated. Meanwhile, millions of unvaccinated residents of lower-income nations like Brazil and India are enduring lethal surges of COVID-19. Crematoriums in Delhi have reached capacity. Less than three percent of Nigeria is vaccinated. São Paolo began exhuming its dead to clear the way for the bodies of new COVID-19 victims. This startling contrast reflects a broader global trend of burgeoning “vaccine deserts” in which no one — not even frontline health care workers — has access to a single dose of the vaccine.
“At the peak of the pandemic in India, I constantly saw catastrophic headlines of new global records of COVID cases and deaths in India while seeing pictures of graduation parties on social media of my American friends. This stark difference in what was going on in my home country versus where I currently live was devastating to see,” Harvard undergraduate Devangana Rana told the HPR. She is originally from Himachal Pradesh, a state in northern India, and she later moved to Urbana, Illinois. If these stark vaccine inequities persist, the poorest countries in the world will not be able to vaccinate most of their populations for at least two years and likely longer — simply because they could not afford to make enormous payouts to drug companies at the early stages of the pandemic. A Gavi official said in an interview, “In a global pandemic, where nobody is safe until everyone is safe, increasing coverage across the entire world ought to be the first priority…by ensuring all countries are able to gain access to life-saving vaccines.” Pandemic surges in lower-income countries and the circulation of potential COVID-19 variants will only stall the entire world’s progress in fighting the pandemic.
As of late October, the U.S. has already administered over 410 million vaccine doses. Though the Biden Administration has already dispatched relief tools and equipment abroad and committed to waiving vaccine patents, these approaches will be most beneficial in the long term. Now, for the greatest impact, the U.S. must accelerate donations of its surplus vaccine doses to poorer countries in dire need.
Correction (February 27, 2024): This article was updated to reflect a different level of attribution offered to one of the interviewees.
Image Credit: Image by Martin Sanchez is licensed under Unsplash License